How to Cure a Yeast Infection Naturally
What is a Vaginal Yeast Infection?
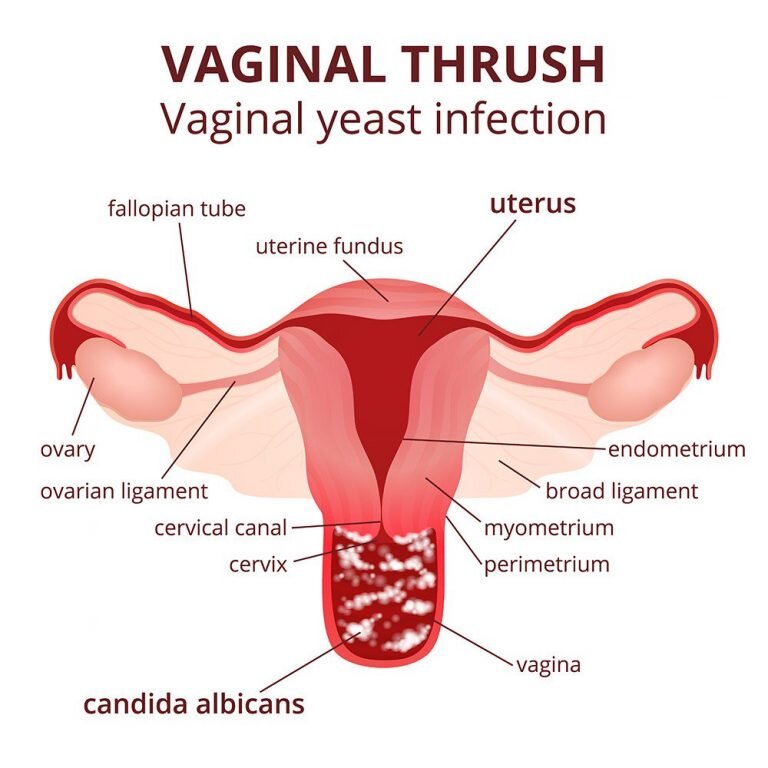
A vaginal yeast infection is an infection of the vagina, most commonly due to a fungus known as Candida. It is known in the medical community as vulvovaginal candidiasis (VVC). At least 75% of women will have a yeast infection at some point in their lives, with nearly 45% experiencing two or more in their lifetime, and 5-8% having recurrent episodes ( a condition known as RVVC, and is defined as four or more episodes within one year). Although they are not life-threatening in women with a healthy immune system, they can greatly impact the quality of a woman’s life, especially in chronic cases. The symptoms range from very mild to severe, and although they are not officially considered an STI, they can be transmitted between sexual partners and to children at birth. Therefore, it is important to understand how to properly treat them.
Signs and Symptoms of Vaginal Yeast Infections:
Yeast infections can have a broad range of presentations, ranging from women who have colonization of yeast but no symptoms to those who have frequent, recurrent, symptomatic episodes.
Here is a list of the most common signs and symptoms:
Vaginal and labial itching and burning
Redness and swelling of the vulva
Abnormal vaginal discharge: This can range from a slightly watery, white discharge to a thick, white, chunky discharge resembling cottage cheese. Note: Most women have some sort of discharge throughout the month, especially during ovulation. However, if you notice any changes or have any questions regarding discharge you are seeing, it is important to contact your doctor right away, as a change in vaginal discharge could indicate something more serious.
Pain with intercourse
Painful urination
Red rash surrounding the vagina and extending toward inner thighs
Symptoms of VVC are often worse the week before your period, with some relief experienced after the onset of menstrual flow. Symptoms of a vaginal yeast infection can include all or only a couple of these symptoms, so it is important to contact your doctor as soon as possible if you notice any of the above changes.
How Do I Know For Sure That It’s Yeast?
This is a very good question. Unfortunately, because many women are hesitant to contact their doctor regarding vaginal symptoms, they will try to diagnose themselves. This results in frequent misdiagnosis and can create more serious consequences, especially if the cause of vaginal symptoms is something that requires a different treatment, such as chlamydia or gonorrhea. For example, although VVC is often assumed to be the cause of vaginitis, only 33% of cases are actually due to VVC. Furthermore, even if it is a yeast infection, over the counter anti-yeast infection treatment does not work for everyone and can lead to chronic Candida infections. Therefore, it is crucial to have a doctor diagnose your vaginitis as being the result of a yeast infection before attempting to treat yourself for this condition.
The greatest concern with self-diagnosis and self-treatment is of women who have recurrent VVC (RVVC). Approximately 5% of women have four or more vaginal yeast infections per year. The danger with self-diagnosis and self-treatment of RVVC is that when women try to treat themselves for what they think is a simple vaginal yeast infection, the underlying cause of their infection may go undiagnosed.
Some of the underlying causes for RVVC include:
HIV/AIDS
Addison’s Disease
Cushing’s Disease
Hypothyroidism or hyperthyroidism
Leukemia
There are also a number of predisposing factors for RVVC that are the same for VVC, and are listed later on in this article.
Note: If you have had a yeast infection diagnosed by a doctor in the past, are certain you are having the same symptoms, do not have recurrent yeast infections, are not pregnant, and have no concern about having acquired an STI, then treating yourself for a yeast infection is probably ok.
How a Doctor Determines You Have Yeast:
Yeast Viewed Through speculum: In order to determine if you have a vaginal yeast infection, your doctor will need to take a thorough history, as well as do a visual inspection of the area. This requires a pelvic examination, which may show swelling and redness of the skin of the vulva, in the vagina, and on the cervix, as well as vaginal discharge consistent with yeast. However, some women have no vaginal discharge or one that appears normal. Your doctor may also notice discreet, pustulopapular peripheral lesions, and cracks in the skin of your vulva. Vaginal pH will be normal (3.5-4.5). As your doctor examines your vaginal canal with the use of a speculum, he or she may also notice a whitish, adherent discharge, although some women may have normal-looking mucus.
In order to confirm a diagnosis of yeast, your doctor may examine a small amount of vaginal discharge under a microscope and/or take a vaginal culture to be analyzed by a lab.
Note: It is becoming increasingly common that even health practitioners are misdiagnosing yeast infections. For example, the most candida-specific criterion for VVC is itching without discharge, but with criterion alone, only 38% of patients actually have VVC.
What Causes Yeast Infections:
Candida albicans is a fungus and is responsible for 85% to 90% of vaginal yeast infections. Other species, such as C. glabrata, C. tropicalis, and C. krusei can also cause vulvovaginal symptoms and tend to be resistant to conventional therapies, such as Monistat and Diflucan. Of the nonalbican species, C. glabrata is the most common.
There are also a number of predisposing factors for VVC, including:
Hormone inbalance
Antibiotic use
Estrogen therapy
Cytotoxic drugs
Contraceptive devices
Hormonal birth control
Immunosuppressive drugs
Chemotherapy/Radiation
Pregnancy
High sugar diet
Food sensivities
Non-cotton underwear
Although the sexual transmission of candida is still controversial, there is evidence to suggest that sexual transmission might be a likely source for recurrent infection. Furthermore, men do get yeast infections on their penis from having sex with a woman with a yeast overgrowth. Therefore, I think it is safe to speculate that if that man does not have that infection treated, he could give it back to his partner. Research has also shown that male sexual partners of women with RVVC had the same strains of candida as their partners. One study also found reservoirs of infection in the oral cavities of 36% of 33 heterosexual couples, the rectums of 33% and the ejaculate of 15% of the men. These results suggest that oral-genital contact is a probable method of sexual transmission.
Conventional Treatment:
The conventional medical approach to the treatment of VVC includes the following:
Fluconazole (Diflucan), Nystatin: These are prescription oral anti-fungal medications. Although these drugs are effective in treating 80-90% of yeast infections, they have a number of known side effects, and may actually promote more yeast overgrowth. They should always be taken with probiotics. Furthermore, the species other than Candida albicans are typically resistant to them.
Topical Anti-Fungal Medication: There a number of over-the-counter medications available for the treatment of VCC. Although they are relatively effective in the treatment of a simple yeast infection due to Candida albicans, the other species of Candida are mostly resistant to these medications. The list of some of the available medications include: butoconazole (Femstat 3), clotrimazole (Lotrimin), miconazole (Monistat), terconazole (Terazol 3).
Naturopathic Treatment Approach:
Although treating the local symptoms of a vaginal yeast infection may be warranted in an acute case, in general, naturopathic doctors treat the gastrointestinal system as well as the vagina when utilizing a VVC protocol. This is due to the fact that clinical evidence has shown that women with yeast infections are also suffering from concurrent gastrointestinal issues and if those are not addressed properly, the yeast infection in the vagina will never resolve completely. Furthermore, a 1977 study demonstrated that in 98 women with RVVC, candida was always found in the feces of those women currently experiencing a yeast infection and not in the women who did not currently have symptoms. In addition, factors that determine a woman’s susceptibility to vaginitis, such as vaginal pH and microflora, vaginal immune tissue and hormonal cycles are all influenced by our general health and dietary habits. This understanding is crucial in the successful management of VVC and especially in managing cases of RVVC.
First Steps:
Get the Symptoms Under Control: There are a variety of way to treat the symptoms of a yeast infection. Below are listed some of the most effective suggestions for women who are not pregnant:
ripe garlic fruits with green parsley leaves isolated on white background
Garlic Oral Supplementation and Vaginal Suppositories: Garlic extracts contain a component called allicin, which inhibits the growth of Candida albicans by blocking the lipid production. It is an excellent antifungal agent. When choosing a form of garlic for oral supplementation, the garlic product with the highest amount of allicin in its stable form should be chosen. A garlic clove can also be inserted into the vagina to kill the yeast off locally. Peel the garlic clove carefully, so as not to nick it, and insert it vaginally at bedtime for 6-8 hours. You can also thread the garlic like a necklace for easy removal. Otherwise, the garlic may occasionally be harder to remove. Relax. It is in there somewhere! In all seriousness, it can sometimes tuck itself behind your cervix. Bearing down as if you are having a bowel movement while searching for it usually does the trick.
Vaginal and Oral Probiotics: Several species of lactobacillus populate the vagina. There are several explanations for why lactobacillus does such a remarkable job at treating vaginal yeast infections. Firstly, lactobacilli produce lactic acid, which contributes to the low (acidic) pH of the vagina. Having an acidic vaginal pH is essential for maintaining a healthy flora and problems arise when the pH becomes more basic. Research has shown that vaginal infections are associated with a decreased amount of vaginal lactobacilli, so it seems logical that vaginal insertion of lactobacillus would be a good treatment for VVC. Secondly, vaginal lactobacilli produce hydrogen peroxide which is a known antibacterial agent. Therefore, lactobacilli act directly as antibacterials and may act as a local immune stimulant in managing microbial levels in the vagina.
The following factors have been shown to reduce the amount of lactobacilli in the vagina:
Sperm
Nonoxynol-9
Frequent oral sex
Douching
Alkaline environment
Racial differences
Menses
Menopause
Furthermore, studies have shown that women with hydrogen-producing lactobacilli in their vaginas are less likely to have Candida vaginitis or bacterial vaginosis. There are a variety of studies showing the efficacy in Candida prevention with oral supplementation of lactobacilli strains. Lastly, a 2003 study reported that oral or vaginally administered lactobacillus is able to colonize the vaginal
ecosystem and that supplementation is necessary for 2-6 months in order to sustain colonization. Lactobacillus rhamnosus has been established as the most effective strain of lactobacillus for both prevention and treatment of VVC and RVVC and seem to be equally as effective if taken orally or vaginally.
Goldenseal (Hydrastis canadensis) and Oregon Grape Root (Berberis vulgaris): Both of these herbs contain berberine, a substance that acts as both an immune enhancer and an antibacterial agent. The immune effect of berberine is especially specific to epithelial mucus membranes found in the mouth, stomach, and vagina. Berberine has also been shown to possess antimicrobial activity against Candida albicans. Goldenseal and Oregon Grape can be prepared for both oral and vaginal supplementation.
Boric Acid: Based on both the research I have done and on clinical results, I would state that this is the most efficacious treatment for VVC and RVVC, especially in combination with the use of appropriate probiotics. Both laboratory tests and human trials support the use of boric acid for the treatment of both Candida glabrata and albicans, even in cases that are resistant to anti-fungal prescription drugs. Studies have shown up to a 98% efficacy rate with the use of boric acid in recurrent vulvovaginal candidiasis (RVVC). Boric acid is extremely effective in treating VVC, RVVC and in the prevention of VVC. In one study comparing boric acid to Nystatin, the boric acid cured 92% after 10 days, and 72% after 30 days, compared to Nystatin, which cured 64% and 50%, respectively. The only side effect noted is slight burning during urination in cases where the infection has already irritated the tissue. This can easily be managed through the use of topical vitamin E.
Zinc: Zinc plays a crucial role in immune function. Therefore, sub-optimal zinc levels can make a woman more susceptible to VVC. Furthermore, one study found significantly lower plasma zinc levels in women with RVVC than in controls.
Homeopathic Remedies: There are a variety of homeopathic remedies that can be used to treat VVC and RVVC.
Ozone Therapy: Major Autohemotherapy is a form of ozone therapy that is an excellent option for stubborn chronic yeast infections that may not respond to other treatment. This should only be performed by a qualified ozone therapist. Vaginal insufflations are another alternative.
Whole-Body Approach:
Avoid Sugar: Numerous practitioners have noticed that in many women with a history of RVVC, consumption of even a small amount of sugar can trigger a yeast infection, and for women with an acute yeast infection, sugar consumption can certainly make it linger longer. One of the theories behind this is that yeast feed off sugar and will only get worse if you eat it. Hopefully, this sensitivity can be reduced after proper treatment of RVVC, however, I would suggest a complete avoidance of sugar during treatment and as much as possible for prophylaxis. Sugar consumption has been linked to a whole host of ailments other than VVC, so it is wise to avoid it for optimal health and well being.
Eliminate Food Allergens: Allergic reactions appear to target the vulvovaginal mucosa in susceptible women, and food allergens can cause irritation in the gut and can lead to the overgrowth of Candida. A Candida overgrowth in the gut can very easily lead to a Candida overgrowth in the vagina. Therefore, eliminating food allergens can make a significant difference in the treatment of yeast infections.
Alcohol: There are a number of reasons to avoid alcohol. With regards to Candida, most alcohol is mainly sugar, which feeds the yeast and makes it worse.
Refined Carbohydrates: The consumption of carbohydrates in general raises your blood sugar and feeds Candida, with refined carbohydrates being the worse culprits. Therefore, it is advisable to avoid refined carbohydrates and significantly reduce your consumption of carbohydrates in general.
The most appropriate way to receive an accurate diagnosis for your symptoms is to see a licensed healthcare practitioner who is familiar with the clinical picture of yeast infections, can perform a gynecological exam, knows what to test for, and can properly collect samples during your exam. If you are certain of what kind of infection you currently have, you can attempt home treatment, but be sure to recognize if your home treatment isn’t working and seek professional care at that time. It is also important to seek professional treatment if you have yeast infections that occur more than three times per year, if you have a chronic yeast infection that will not resolve, or if you are pregnant.
With patience, motivation and proper medical care, even the most most stubborn yeast infections can be successfully treated!
References:
Pubmed Health
Medicinenet
WebMD
Women’s Encyclopedia of Natural Medicine: Tori Hudson
Nutritional Medicine: Alan Gaby